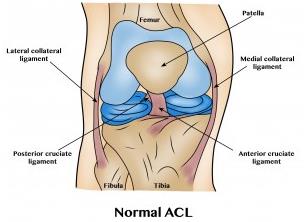
The ACL
The ACL is one of the four main ligaments within the knee that connects the femur to the tibia. It runs diagonally in the middle of the knee, preventing the tibia from sliding out in front of the femur, as well as providing stability to the knee.
ACL ruptures are often the result of pivoting, sidestepping or twisting movements, and approximately half of ACL injuries occur in combination with damage to the meniscus, articular cartilage, or other ligaments. Additionally, patients may sustain bruising to the bone beneath the cartilage. An MRI is often required to diagnose the injury, and close clinical follow-up is needed to facilitate a rehabilitation and return to daily activities.
Treatment for an ACL rupture can vary depending on the patient’s activity level, degree of injury, and instability symptoms. ACL reconstruction is almost always an elective procedure, and some patients may opt to continue without surgery.
The main reason for an ACL reconstruction is to prevent instability that can become apparent after an ACL rupture. If reconstruction is being performed it’s important to prepare the knee ensure an optimal outcome, namely reducing swelling and gaining full extension and flexion of the injured leg. Patients who lack full extension or who have a stiff, swollen knee at the time of surgery may have significant problems regaining motion after surgery.
Surgical Treatment
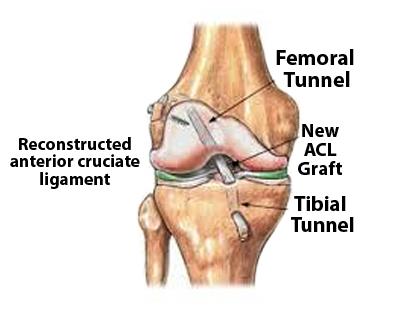
ACL reconstructions involve replacement of the torn ligament with a substitute graft made of tendon. This autograft tendon is often taken from the patient’s own patella, hamstring or quadriceps. In some circumstances where an autograft tendon is not available, an allograft tendon (taken from a cadaver) is used.
Surgery is performed under general anaesthetic, and the area is infiltrated with local anaesthetic as well. You will be left with one vertical or oblique scar on the front of the knee together with two small portal scars where the arthroscope instruments have entered the knee. You will be awake shortly after surgery is complete, and on return to the ward a cuff filled with ice and cool water will be applied to your knee to help control swelling. Two drains may also be placed into the knee joint so that unwanted blood does not accumulate. These are removed after 6 hours.
You will normally go home the morning or day after surgery, although in some cases the surgery is performed as a day procedure. You will be given information on discharge about rehabilitation which can be undertaken either under the supervision of a physiotherapist or on your own.
Patient Information
This page is available to download as an information sheet.
-
Pain Management
After your surgery it’s likely that you will feel some discomfort. This is part of the healing process. The local anaesthetic will wear off over 8 hours, and medications are often prescribed for short-term pain relief. Along with further over-the-counter analgesics a combination of rest, ice, compression, and elevation is very important during the early days of your recovery.
-
Rehabilitation
The main aim is to restore full extension of the knee.
A physiotherapist will visit you while you are in hospital to talk about exercises and to help you straighten your knee. They will also help you regain quadriceps function as well as make sure you are confident with your crutches. It is generally not necessary to see a physiotherapist during the first two weeks after surgery, however you should follow the instructions given to you at discharge with regard to gentle range of movement exercises. It is beneficial to see a physiotherapist to help guide your rehabilitation, particularly if you plan to return to sport.
A brace or splint is usually not required.
-
Post-Surgery
How much time you require off work will vary on the type of work you do. As a general rule sedentary work can be undertaken again after two weeks. Heavy manual work may be anywhere from 2-3 months. For a more accurate idea of how much time you will need off work speak to your surgeon.
In general crutches are required for up to 2 weeks.
With regard to returning to sport, most patients are able to return to some of their activities at 4 months post-surgery. By 6 months most patients can gradually resume training for sport with the view to return to play at 12 months. Improvement will continue for a further 6-12 months after that.
For more information about ACL surgery and recovery see acltear.info for more information. -
Complications
While most patients are happy with the outcome of their surgery, there are always some risks involved that need to be addressed.
-
Infection
The incidence of infection after arthroscopic ACL reconstruction is very low. Antibiotics are given at the time of surgery to reduce the risk, however despite this infection of the wound can occur. This is usually easily treated with antibiotics. Unfortunately, sometimes the infection gets into the joint and this is a serious complication requiring admission to hospital, intravenous antibiotics and sometimes surgery.
-
DVT
A thrombosis is a blood clot that forms in the veins in the legs. This can cause persistent swelling of the foot and ankle and can dislodge and be carried to the lungs, resulting in chest pains and breathing difficulties.
-
Donor Site
If you had a hamstring graft it’s common to experience a tearing sensation at the back of the knee approximately 3-6 weeks post-surgery. This is a stretching of the scar tissue at the harvest site and although it can be associated with some pain and swelling, this usually settles after a few days.
-
Re-rupture
The risk of re-tearing a previously repaired ACL graft is approximately 15% higher than normal.

